Nuss Procedure
Key Terms:
Invasive Surgery: An surgery that breaks the skin, like one that requires incisions or needles. Similarly, a non-invasive surgery does not involve tools that break the skin. A minimally-invasive surgery involves smaller incisions, and shorter recovery time than invasive surgery [1].
Sternum: A flat bone that lies in the middle front part of the rib cage, sometimes called the breastbone. In more complicated words, the breastbone "is a partially T-shaped vertical bone that forms the anterior portion of the chest wall centrally" [2]. In pectus excavatum, the breastbone is sunken into the chest.
What is the Nuss Procedure?
The Nuss Procedure is an minimally-invasive procedure used to surgically correct pectus excavatum. It works best for kids who have passed puberty but haven't reached adulthood, when the bones are still malleable and the pectus has stabilized. It has also been preformed in adults successfully [3]. The Nuss procedure uses a stainless steel bar to push the breastbone forward. It's considered a "minimally invasive" procedure because typically only three small incisions are needed (one for the camera and two for the bar), although it is an intensive and painful surgery [4].
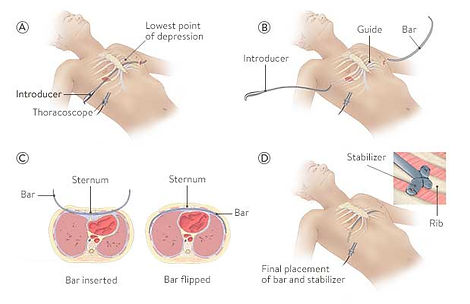
Image showing the steps of the Nuss procedure
Nuss procedure [Illustration]. (n.d.). https://www.stanfordchildrens.org/en/service/chest-wall/pectus-excavatum
What you should know
What happens during the procedure?
1. A concave stainless steel bar is slipped under the sternum with the assistance of a small camera, called a scope, using two incisions made on each side of the chest.
2. The bar is flipped, and the sternum is moved to the proper position.
3. To keep the bar from moving, a metal plate called a stabilizer is inserted on one or both sides of the chest. The stabilizer fits around the bar and into the ribcage where it is secured in place. [4]
In some cases, two bars can be used to correct the pectus. In a study of 1,215 patients who underwent the Nuss procedure, 1 bar was placed 49.8% of the time; 2 bars, 49.4%; and 3 bars, 0.7% [5]. Patients with symmetric or mild pectus typically receive one bar, and patients with asymmetric or severe pectus typically receive two or more [8].
Does the bar come out? How long does it stay in?
Yes, the Nuss bar isn't permanent. Most surgeons and institutions advise that the bar stay in for three years [9][10]. The removal process is significantly easier than the insertion process. In comparison to the surgery for insertion, which typically requires somewhere around 3 days in the hospital, recovery from the removal process often only requires between 3 and 6 hours in the hospital. Removal is also a lot easier to recover from and doesn't need as long of a recovery process [14].
How long is the recovery process for the insertion of the bar?
Recovery for the Nuss procedure is very difficult. Most patients begin feel back to normal by around the 3 week mark, although they can only begin driving around the six week mark, begin contact sports by the three month mark, and they may still feel the bar moving or shifting up until the six month mark [11].
The Nuss procedure typically takes around 2 hours, but it can last up to 4 hours in more complicated cases. [6] [7]


X-Ray of the Nuss bar after the Nuss procedure
What's the recovery process like? How long would I stay in the hospital after surgery if I had the Nuss procedure?
After surgery, you'll stay in the hospital for three to four days to help manage pain while the you recover [3]. While in the hospital, physical therapy will help the you walk and use the bathroom (after the catheter is removed). The recovery process is very painful and difficult, but the hospital that preforms this procedure will have a strong painkiller regimen to help decrease the pain []. The specific medications used will vary between hospitals and surgeons. After the procedure, you probably won't want to get out of bed, but movement is vital to the recovery process.


What the Nuss bar looks like
Is there any chance the pectus could come back after the bar has been removed?
It's very uncommon, there's roughly 1 to 2% chance that the pectus could come back after bar removal. Even if there was a regression, it's unlikely that the pectus would return back to its previous depth. [13] [14]
What are the complications associated with this procedure?
1. Bar displacement: Occurs in less than 1% of cases [17].
2. Pneumothorax (collapsed lung)
3. Wound seroma (a fluid build-up in an area after surgery)
Every procedure has risks, but the Nuss procedure is a safe, standardized procedure with a low complication rate,
The risk of complications is higher in adults [18].
What do I need to do to get the Nuss procedure?
-
Find a hospital that performs the Nuss procedure.
-
Testing is vital to the surgery process, the hospital you're thinking of getting the procedure at will want to make sure you're a good candidate for the surgery. Start by making an appointment with your child's pediatrician or primary care physician; he or she will help you find where to get these tests. Most hospitals will ask for the results of the following tests: [19]
-
Thoracic CT or Thoracic MRI (to measure your Haller Index)
-
Echocardiogram
-
EKG
-
Metal allergy testing (to make sure you won't be allergic to the bar)
-
Pulmonary function test
-
-
Research surgeons. The right surgeon can make a big impact on your experience and the appearance of your pectus after surgery.
-
Make an appointment for a consultation. The hospital team at the hospital you've selected will help make a care plan for you.
Does this treatment have any impact to the body that's relevant to pregnancy?
The treatment does not have any impact on future pregnancies or risk to becoming pregnant. [14]
How long does the procedure take?
Tips
What are the must-have items for the
procedure?
-
Triangle wedge pillow - Vital. At night, patients can use their triangle pillow to prevent rolling to the side. Side or stomach sleeping generally isn't advised for the first four weeks after surgery, and in addition, most patients find side sleeping painful after surgery. During the day, the pillow can be used to prop up the patient at an angle. [22]
-
A recliner - A wedge pillow can substitute for a recliner. A recliner is helpful after the surgery because it allows the entire body to be supported, from the feet to the head. Some people may feel more comfortable sleeping in a recliner chair the first few days after surgery. [22] [16]
-
Clothes that zip up or are easy to put on - Because patients cannot raise their arms above their head after their procedure for some time, tops they can put on that can zip or are loose will be absolutely necessary. [21] [22]
-
Heating pad - Heating pads are fantastic for relaxing the body and reducing pain after the Nuss procedure. [21] [15]
Are there any surprises?
-
Coughing, sneezing, and laughing hurts a lot for most patients while they recover. However, it's temporary and goes away during the following weeks [15].
-
Getting up and lying down is surprisingly painful. The easiest and most painless way to lie down is to have someone hold the patient's back and have them lower the patient down [15].
-
Muscle atrophy is a major issue. Walking, posture training, weight training and calisthenics (light weights can be used around week 4) are all vital to the recovery process. Just keeping the head up or sitting at the kitchen table can be difficult in the first weeks after surgery. Major muscle atrophy can be prevented by staying active [12] [20] [21].
-
Depending on the deepness of the patient's pectus, they can experience stretching of the skin in the area of their pectus as the skin accommodates the new shape of the chest. The temporary thinness of the skin in the area of the breastbone might be uncomfortable for the patient, but Aquaphor, Vaseline, or similar lotions make a great fix.


What pectus looks like before the Nuss procedure
What's the timeline for the recovery process?
Day 0
Day 1
Day 2
Day 3
Week 1
The Nuss procedure is an intensive surgery with a long recovery process [7]. Timelines can very from hospital to hospital. The following information is compiled from the Nuss Center at the Children's Hospital of the King's Daughters in Norfolk, Virginia. Following the procedure, the recovery timeline can be divided into milestones: Days 1, 2, 3; Weeks 1, 2-3, 4; and Months 2 and 3. [11] [12]
Surgery Day. Today's goal is rest and pain management. You will also need to begin using your incentive spirometer (a plastic device that measures your breathing, like an exercise machine for the lungs) to encourage deep breathing.
.
Your catheter will be removed. Physical therapy (PT) will work with you to help you get out of bed, use the bathroom, sit in a chair, and walk.
Goals: Try to walk two times today with a PT.
This is often the hardest day for the patient, because they are coming off the heaviest drugs.
Goals: Go up and down stairs with PT and do some walking on your own.
This is typically the day patients are discharged.
-
Stay at home to avoid physical contact with people, but try to stay active, don't sit in your bed all day. Try to get some walking in, it is vital to the recovery process.
-
Walk several times a day and use your incentive spirometer.
-
Starting weaning off medication. When it becomes possible, avoid waking up for overnight medications.
-
You can raise your arms to wash or comb your hair, but not for prolonger overhead reaching
-
Limit lifting to 5 pounds
-
You should sit in the backseat when traveling to avoid airbags.
-
The patient can return to work or school as long as they are no longer taking opioid pain medication or muscle relaxants.
-
Incisions should be mostly healed. If the Steri-Strips haven't fallen off after three weeks, you can remove them by gently rubbing them off with a washcloth or by using rubbing alcohol. If they are still well attached, it's ok to leave them on and allow them to fall off on their own.
-
Swelling should have mostly subsided by this point. You might be able to see or feel the pectus bar by this point.
-
Focus on posture excercises.
-
You can begin to raise your hands above your head.
-
You should be off all medications, including opioids, except ibuprofen (Motrin) or acetaminophen (Tylenol)
-
Remember to sit in the backseat of any vehicle to avoid airbags
-
You can begin to sleep on your side or stomach.
-
You can twist at the trunk.
-
You can carry a backpack.
-
You can begin to drive and return to the passenger seat.
-
Continue to avoid heavy lifting, but you can begin light calisthenics and jogging.
-
We highly recommend that you begin light upper body weight training - no more than 2 to pounds.
-
You may return to contact sports like basketball baseball, soccer, etc.
-
You can participate in physical education at school.
-
The bar stops all movement or shifting.
Week 2
Week 4
Month 2
Month 3
Month 6
What medications will be used?
Different hospitals or centers will advise different medications and pain management. Here is a sample pain management and medication plan from the Children's Hospital of the King's Daughters, in Norfolk, Virginia.
-
It is normal to require some opioids for 1-2 weeks after surgery.
-
In general, patients will use Tylenol/Ibuprofen/Robaxin around the clock, and then continue during waking hours for an additional 1 to 2 weeks.
-
The pain from surgery is usually worse a night-time, so the night-time dosing should be weaned last. A good night's sleep is very important, if possible, avoiding waking up at night to take medication.
-
Valium can be added if narcotics are not relieving pain, especially when pain is more "muscle spasm" in nature.
-
One thing to be wary of is that the opioid and Valium, when given together, may be particularly sedating, so this is a combination best separated in timing during the day but acceptable during the night.
-
Avoid taking any medications on an empty stomach.
-
You will be given a 1 week's supply of opioid medication and a 1 month supply of the other medications at discharge. However, you will probably not need all the medicine that is prescribed.
Oxycodone (or equivalent opioid) - primary pain reliever
We anticipate you needing to take this for approximately 2 weeks total, including time to completely wean this off.
Robaxin (Methocarbamol) - muscle relaxant
We recommend that you take this at least in the morning when you wake up and at night before you go to bed to help with stiffness. It doesn't have the sedating effect of Valium.
Advil/Motrin (Ibuprofen) - non-steroidal anti-inflammatory
It is recommended that you take this medication with at least 8 oz of water or milk in order to prevent stomach upset.
Tylenol (Acetaminophen) - non-opioid analgesic
Valium (Diazepam) - muscle relaxant
Good for acute, severe muscle spasms, can be somewhat sedating, helps with anxiety.
Colace (stool softener) AND Miralax (laxative)
Constipation is a common side effect of opioids, so dosing of Colace and/or Miralax is recommended, as is consuming adequate quantities of water.
Zofran (Ondansetron) - for preventing nausea and vomiting
Scopolamine transdermal patch - Can be placed before the surgery, may be used to prevent nausea from anesthesia
Phenergan - May be used to prevent nausea from anesthesia for some patients
References
1. Minimally invasive surgery. (n.d.). Yale Medicine. https://www.yalemedicine.org/
conditions/minimally-invasive-surgery
2. Altalib AA, Miao KH, Menezes RG. Anatomy, Thorax, Sternum. [Updated 2023 Jul 24].
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK541141/
3. Nuss procedure. (n.d.). Children's Hospital of Philadelphia. Retrieved November
5, 2023, from https://www.chop.edu/treatments/
nuss-procedure#:~:text=The%20Nuss%20procedure%20is%20a,until%20the%20age%20of%201
9.
4. Casas-Melley, A. (n.d.). Pectus excavatum: The Nuss Procedure. Kids Health.
Retrieved November 6, 2023, from https://kidshealth.org/en/parents/
nuss-procedure.html
5. Kelly, R. E., Jr, Obermeyer, R. J., Goretsky, M. J., Kuhn, M. A., Frantz, F. W., McGuire, M. M., Duke, D. S., Daniel, A., & Nuss, D. (2022). Recent Modifications of the Nuss Procedure: The Pursuit of Safety During the Minimally Invasive Repair of Pectus Excavatum. Annals of surgery, 275(2), e496–e502. https://doi.org/10.1097/SLA.0000000000003877
6. What to Expect: The Nuss Procedure [Pamphlet]. (n.d.). Texas Children's
Hospital. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/
https://www.texaschildrens.org/sites/default/files/uploads/documents/
NussBarGuide_2021_v33.pdf
7. Nuss procedure. (n.d.). Cleveland Clinic. https://my.clevelandclinic.org/health/
treatments/22635-nuss-procedure
8. Ben, X. S., Deng, C., Tian, D., Tang, J. M., Xie, L., Ye, X., Zhou, Z. H., Zhou,
H. Y., Zhang, D. K., Shi, R. Q., Qiao, G. B., & Chen, G. (2020).
Multiple-bar nuss operation: An individualized treatment scheme for
patients with significantly asymmetric pectus excavatum. Journal of
Thoracic Disease, 12(3), 949-955. https://doi.org/10.21037/jtd.2019.12.43
9. Pectus Excavatum FAQs. (n.d.). Medical University of South Carolina.
https://musckids.org/our-services/surgery/chest-wall-deformity-center/
pectus-excavatum/
pectus-excavatum-faq#:~:text=The%20brace%20(pectus%20bar)%20will,in%20place%20for
%20three%20years.
10. Park, H. J., & Kim, K. S. (2016). Pectus bar removal: Surgical technique and
strategy to avoid complications. Journal of Visualized Surgery, 2, 60.
https://doi.org/10.21037/jovs.2016.02.27
11. Children's Surgical Specialty Group - Pediatric Surgery Pectus Excavatum/
Carinatum Enhanced Recovery after Surgery [Pamphlet]. (2018). Children's
Hospital of the King's Daughters.
12. Nuss Procedure - Post Surgery Daily Goals [Pamphlet]. (2023). CHKD Nuss Center.
13. Cho, D. G., Kim, J. J., Park, J. K., & Moon, S. W. (2018). Recurrence of pectus
excavatum following the nuss procedure. Journal of Thoracic Disease,
10(11), 6201-6210. https://doi.org/10.21037/jtd.2018.10.31
14. Olson, E. (2023, April 24). [E-mail interview].
15. Ehrich, P. (2022, June 22). Recovering from the Nuss Procedure: Tips from the
Patient Perspective. Children's Hospital of the King's Daughters.
https://www.chkd.org/blog/
recovering-from-the-nuss-procedure--tips-from-the-patient-perspective/
16. Going home after a Nuss procedure. (n.d.). Phoenix Children's Hospital.
chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/
https://www.phoenixchildrens.org/files/inline-files/NUSS%201674.pdf
17. Nuss, D. (2008). Minimally invasive surgical repair of pectus excavatum.
Seminars in Pediatric Surgery, 17(3), 209-217. https://doi.org/10.1053/
j.sempedsurg.2008.03.003
18. Akhtar, M., Razick, D. I., Saeed, A., Baig, O., Kamran, R., Ansari, U., Sajid,
Z., & Rahman, J. E. (2023). Complications and outcomes of the nuss
procedure in adult patients: A systematic review. Cureus. https://doi.org/
10.7759/cureus.35204
19. Patient Evaluation Guidelines. (n.d.). Children's Hospital of the King's
Daughters: Nuss Center. http://chkd.wsoldev.com/our-services/nuss-procedure/
nuss-procedure-patient-evaluation-guidelines/
20. Lyon, K. (2023, October 7). [Personal interview by the author].
Dr. Katy Lyon, PT, DPT, is a physical therapist at Back in Motion Physical Therapy, in Lorton, Virginia.
21. Hathaway, A. C. (2023, December 18). [Online forum post]. Facebook, Pectus
Excavatum Surgeries. https://www.facebook.com/groups/1210391819010011/
permalink/6896037373778732/
Comment by Sara Ashton Weber
22. Victoria, C. (2023, December 18). Hi everyone. My son's PE Nuss procedure is
scheduled for tomorrow. What should I pack for him? [Online forum post].
Facebook: Pectus Excavatum Surgeries. https://www.facebook.com/groups/
1210391819010011/permalink/6896295587086244/