What is pectus?
Overview
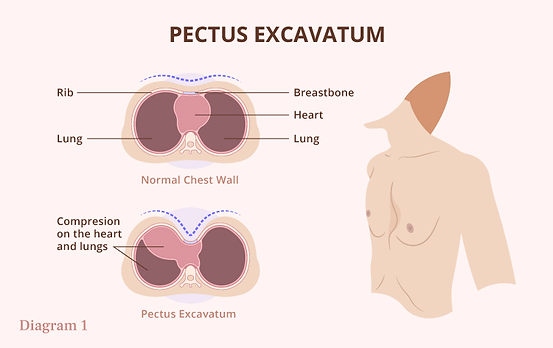
Pectus excavatum is a condition where a person's breastbone is sunken into the chest. In many people, pectus excavatum can look as if the center of the chest has been scooped out, which is why the condition is sometimes called "funnel chest" or "dented chest" [1].
Pectus excavatum is a chest wall deformity. The chest wall is the structure that surrounds the vital organs, made of skin, fat, muscles, and the rib cage [2]. A chest wall deformity is created when the chest wall doesn't develop correctly, creating a structural abnormality of the chest. In pectus excavatum, the breastbone and some of the ribs grow inward, changing the shape of the chest wall and sometimes compressing the internal organs [3].
Some patients with pectus experience chest and back pain, but the exact cause of this pain is poorly understood [17].
Some patients with pectus experience chest and back pain, but the exact cause of this pain is poorly understood [17].
What are the symptoms of pectus? What does it look like?
Pectus can look like the center of the chest has been scooped out, leaving a deep dent around the breastbone area. Many people who have pectus excavatum will also tend to have a hunched-forward posture (kyphosis), with flared ribs and shoulder blades [1].
Pectus is more than a cosmetic condition, it can cause a variety of symptoms [7]. Symptoms of pectus normally are minimal in childhood, increase greatly during adolescence, and then remain constant during adulthood [8]. Severe pectus excavatum can put pressure on the lungs and heart [11], but the severity of the pectus doesn't always match up with the severity of symptoms [18].
Symptoms of pectus excavatum include: [3][1][7]
-
a hollow depression in the chest
-
shortness of breath during exercise
-
chest and back pain
-
tiredness
-
coughing or wheezing
-
dizziness
-
rapid heart rate or heart palpations
What are the effects of pectus excavatum?

Physical effects:
Pectus can compress internal organs like the lungs and heart. For the heart, compression can in some cases stop the heart from filling with blood and pumping it out as fast as it needs to. Pectus has been known to cause unusually fast heart rates (tachycardia), heart murmurs (systolic cardiac murmur), and mitral valve prolapse.
For the lungs, the depth of the pectus indentation can stop the lungs from fully expanding, stopping the person with pectus from taking a full breath. This can decrease the ability of people with pectus to exercise because breathing is difficult. In addition, pectus can cause other symptoms as well [16] [11]:
Fatigue
When exercising, a person with pectus excavatum compensates by engaging the diaphragm while breathing to allow the lungs to expand more and to obtain "adequate oxygen and carbon dioxide exchange for the demands of the body". The additional energy needed to breathe this way causes fatigue, which forces patients with severe pectus excavatum to be less active than their peers as a result. This can be especially difficult for teens, who often step back from sports or other high-stress physical activities [16].
Chest and back pain
Some patients with pectus experience chest and back pain, but the exact cause of this pain is poorly understood [17].
Coughing or wheezing
Dizziness
The compression of the lungs in patients with severe pectus can cause them to cough or wheeze as they breathe [1].
Recurrent respiratory infections
Heart murmurs
Psychological effects:
People with pectus can have low body positivity and low self-esteem because of the condition [12]. Many are so self-conscious about their appearance that they avoid activities where their chest can be seen (like swimming) and clothing that makes their chest visible. Children with pectus are more likely to have psychosocial issues (depression, anxiety, withdrawal, etc.) than children without the condition [13]. Pectus excavatum has been associated with increased social anxiety, low self-esteem, feelings of inferiority, depression, poor body image, shyness, and depression [14] [15]. Some people opt to get surgeries like the Nuss or Ravitch procedures to correct their pectus purely for cosmetic purposes, sometimes because of the teasing or bullying they experience [13].
What causes pectus?
Doctors aren't clear on what causes pectus. However, it sometimes runs in families, so it may be an inherited condition. About 30% to 40% of people with pectus excavatum have a biological family member with the same condition. [11] [4]. Pectus is equally common in boys than in girls, but more boys are diagnosed and referred for surgery than girls, which could partially be the case because of breast tissue that can sometimes hide the condition [19] [20].
Is pectus connected to other conditions?
Pectus has been linked to scoliosis, Ehlers-Danlos syndrome, and Marfan syndrome. For example, pectus excavatum is found in ⅔ of patients with Marfan syndrome. Ehlers-Danlos and Marfan are both connective tissue disorders, which might show a connection between pectus and connective tissue issues. Studies show a pattern of inheritance as high as 37% [6].
Approximately 15 percent of children with pectus excavatum also develop scoliosis (curvature of the spine) [3].
How does pectus develop with age?
Pectus excavatum is a congenital condition, which means that you are born with it. It's often noticeable shortly after birth, but can sometimes remain undetected until puberty. Then, during adolescence, pectus typically becomes more severe, and much more visible [3]. There is limited information about pectus in adults, but doctors do know that pectus persists through adulthood, and often causes worsening symptoms with aging [17] [18].
How do I get a diagnosis for pectus?
Multiple tools are used by doctors to diagnose pectus and its severity [3]:
-
Visual examination of the chest
-
Auscultation (analysis of sounds of the heart and chest to detect the condition's effect on heart and lung function)
-
Electrocardiogram (ECG, also called EKG)
-
Echocardiogram (a noninvasive test that takes a picture of the heart with sound waves)
-
Pulmonary function testing (breathing into a mouthpiece connected to an instrument that measures the amount of air breathed over a period of time)
-
Chest X-ray
-
CT-scan
-
A measure of the severity of pectus excavatum by a CT scan. It's calculated by obtaining the "ratio of the horizontal distance of the inside of the ribcage and the shortest distance between the vertebrae and sternum". A Haller Index of greater than 3.25 is generally considered severe, and a normal Haller Index is 2.5 [3].
Haller Index
References
1. Pectus excavatum. (2022, March 31). Mayo Clinic. https://www.mayoclinic.org/
diseases-conditions/pectus-excavatum/symptoms-causes/syc-20355483
2. Pourtaheri, N. (n.d.). Chest wall anatomy (T. R. Gest, Ed.). Medscape.
https://emedicine.medscape.com/article/2151800-overview?form=fpf
3. Chest wall deformities. (n.d.). Boston Children's Hospital.
https://www.childrenshospital.org/conditions/chest-wall-deformities
4. Creswick, H. A., Stacey, M. W., Kelly, R. E., Gustin, T., Nuss, D., Harvey, H.,
Goretsky, M. J., Vasser, E., Welch, J. C., Mitchell, K., & Proud, V. K.
(2006). Family study of the inheritance of pectus excavatum. Journal of
Pediatric Surgery, 41(10), 1699-1703. https://doi.org/10.1016/
j.jpedsurg.2006.05.071
5. Kotzot D, Schwabegger A H. Etiology of chest wall deformities—a
genetic review for the treating physician. J Pediatr Surg. 2009;44:2004–2011.
6. Blanco, F. C., M.D., Elliott, S. T., M.D., & Sandler, A. D., M.D. (2011,
February). Management of congenital chest wall deformities (K. K. Evans,
M.D., S. Mardini, M.D., & P. G. Arnold, M.D., Ed.). National Institute of
Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3140238/
7. Crump HW. Pectus excavatum—pathophysiology, clinical presentation, surgical repair. Am Fam Physician. 1992;46:173–9.
8. Fonkalsrud, E. Current Management of Pectus Excavatum. World J. Surg. 27, 502–508 (2003).
https://doi.org/10.1007/s00268-003-7025-5
9. Harris, C., Croce, B., & Cao, C. (n.d.). Pectus excavatum - PMC. National
Institute of Health.
10. Adela T. Casas-Melley, A. T. (Ed.). (n.d.). Chest wall disorder: Pectus
excavatum. Nemours KidsHealth. https://kidshealth.org/en/parents/
pectus-excavatum.html#:~:text=Health%20care%20providers%20diagnose%20pectus,echoc
ardiogram%20to%20test%20heart%20function
11. Pectus excavatum. (n.d.). Cleveland Clinic. https://my.clevelandclinic.org/
health/diseases/17328-pectus-excavatum
12. Steinmann C, Krille S, Mueller A, Weber P, Reingruber B, Martin A. Pectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: a control group comparison of psychological characteristics prior to surgical correction. Eur J Cardiothorac Surg. 2011 Nov;40(5):1138-45. doi: 10.1016/j.ejcts.2011.02.019. Epub 2011 Mar 25. PMID: 21440452.
13. Ji Y, Liu W, Chen S, Xu B, Tang Y, Wang X, Yang G, Cao L. Assessment of psychosocial functioning and its risk factors in children with pectus excavatum. Health Qual Life Outcomes. 2011 May 4;9:28. doi: 10.1186/1477-7525-9-28. PMID: 21542911; PMCID: PMC3098203.
14. Roberts, J., Macmath, S., English, M., & Martin, J. (n.d.). BODY DISFIGUREMENT
AND THE QUALITY OF LIFE OF ADOLESCENTS WITH PECTUS EXCAVATUM: EFFECTS OF
THE NUSS PROCEDURE. Retrieved November 5, 2023, from
https://files.eric.ed.gov/fulltext/EJ795474.pdf
15. Closway, L. (n.d.). Mayo Clinic Q and A: Understanding and treating pectus
excavatum. Mayo Clinic. Retrieved November 5, 2023, from
https://newsnetwork.mayoclinic.org/discussion/
mayo-clinic-q-and-a-understanding-and-treating-pectus-excavatum/
16. Pectus excavatum. (n.d.). Columbia Surgery. Retrieved November 5, 2023, from
https://columbiasurgery.org/conditions-and-treatments/pectus-excavatum
17. Jaroszewski, D., Notrica, D., McMahon, L., Steidley, D. E., & Deschamps, C.
(2010). Current management of pectus excavatum: A review and update of
therapy and treatment recommendations. The Journal of the American Board of
Family Medicine, 23(2), 230-239. https://doi.org/10.3122/
jabfm.2010.02.090234
18. Jaroszewski DE, Fonkalsrud E. Pectus deformity in the adult patient: cardiopulmonary symptoms as an indication for repair. Presented at the 27th annual International Scientific Assembly of the American College of Chest Physicians, Salt Lake City, Utah; 2006.
19. Fonkalsrud E. W. (2004). Management of pectus chest deformities in female patients.
American journal of surgery, 187(2), 192–197. https://doi.org/10.1016/j.amjsurg.2003.11.010
20. Aly, M. R., Farina, J. M., Botros, M. M., & Jaroszewski, D. E. (2023). Minimally invasive repair of pectus excavatum in adults: a review article of presentation, workup, and surgical treatment. Journal of thoracic disease, 15(9), 5150–5173. https://doi.org/10.21037/jtd-23-87